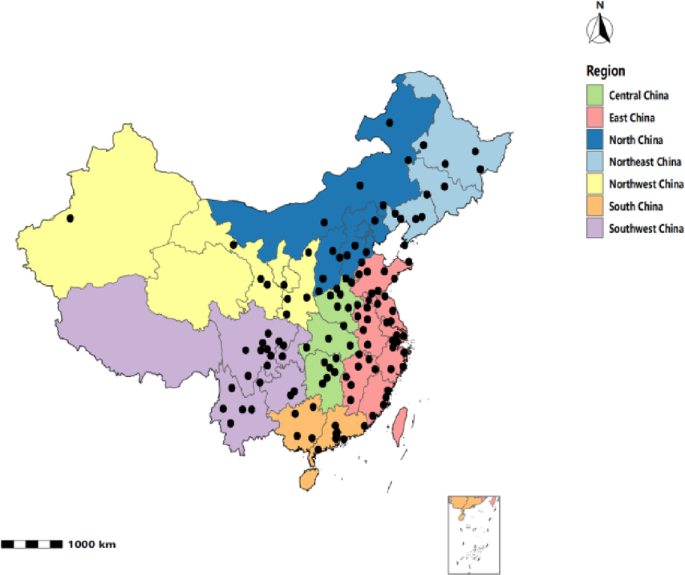
The association between air pollution and cardiovascular health in middle-aged and older Chinese adults: cross-sectional and prospective analyses
This study, drawing on a large sample of middle-aged and older adults from the CHARLS cohort, systematically examined the associations between multiple air pollutants and HD risk. Particulate matter, including PM₁, PM₂.₅, and PM₁₀, was positively associated with cardiovascular events, and these associations remained robust across multi-pollutant models and sensitivity analyses, suggesting that particles of different sizes may exert consistent adverse effects on cardiovascular health. In the cross-sectional GLM analyses, the associations for PM₁₀ were relatively consistent across models; however, the effect size was minimal and of limited clinical relevance.
This finding is consistent with several international studies. A prospective analysis based on the UK Biobank reported that combined exposure to multiple air pollutants may increase the risk of HD, particularly heart failure, with PM₂.₅ and PM₁₀ identified as the main drivers26. Similarly, systematic reviews and meta-analyses have consistently demonstrated significant associations between PM₂.₅ exposure and the incidence of heart failure27,28,29. In the Chinese context, a study using data from the Global Burden of Disease database showed that PM₂.₅-related HD mortality increased steadily between 1994 and 2019, with risks rising significantly with age30. In South Korea, a nationwide cohort study found that long-term PM₂.₅ exposure was associated with higher HD mortality among middle-aged adults, with the strongest associations observed for heart failure–related deaths31. Collectively, this body of evidence highlights the substantial public health burden of particulate matter pollution across diverse populations. In comparison, the present study not only confirmed the robustness of PM₂.₅ and PM₁₀ associations in a nationally representative Chinese sample, but also complements recent time-series evidence showing that short-term PM₁ exposure increases the risk of HD deaths, with approximately 5.7% of related deaths attributable to PM₁, and older adults being disproportionately affected32. Taken together, these short-term and long-term findings suggest that PM₁ may play an important role in the development of HD.
In contrast, the associations of NO₂ and O₃ were less consistent in this study. NO₂ was related to cardiac risk in single-pollutant models, but its effects were unstable in multi-pollutant models. Such inconsistencies were not observed in the European ELAPSE Project, which found that NO₂ remained associated with cardiovascular outcomes even at low concentrations and retained significance in multi-pollutant models33, suggesting that differences in exposure assessment and model specification may partly explain the divergent findings. Results for O₃ were likewise unstable, showing inverse associations in some models but a reversal of direction after adjustment for exposure windows. The ELAPSE Project also reported that associations between O₃ and mortality were substantially attenuated in multi-pollutant models33. Additionally, a cross-sectional imaging study among healthy Canadian adults found that NO₂ was associated with reduced carotid wall volume (CWV), whereas O₃ was significantly associated with increased CWV34, suggesting that gaseous pollutants may affect subclinical atherosclerosis through complex biological pathways. Taken together, our findings and prior evidence suggest that the health effects of NO₂ and O₃ remain uncertain, highlighting the need for future investigations that incorporate more refined individual-level exposure assessments and optimized multi-pollutant modeling strategies. Notably, the inverse associations of O₃ observed in multi-pollutant models should not be construed as protective effects, but are more likely to represent artifacts driven by exposure correlation structures or model specifications.
Beyond epidemiological evidence, a growing body of reviews and experimental studies has elucidated the potential mechanisms linking air pollution to HD. Long-term PM₂.₅ exposure has been shown to elevate the risk of acute coronary syndrome, myocardial infarction, arrhythmias, and heart failure through oxidative stress, systemic inflammation, endothelial dysfunction, autonomic imbalance, and thrombogenesis29,35,36,37. Animal studies further demonstrate that chronic PM₂.₅ exposure induces myocardial structural damage and inflammatory responses, accompanied by increased expression of ICAM-1, CRP, and other inflammation-related proteins38; nanoparticles may also deposit at vascular lesions, accelerating local inflammation and atherosclerosis39. At the molecular level, air pollution promotes reactive oxygen species (ROS) generation and activates key signaling pathways—including Toll-like receptors (TLRs), NF-κB, Nrf2, and the aryl hydrocarbon receptor (AhR)—thereby triggering inflammatory and oxidative stress responses40,41,42,43. These processes impair vascular relaxation, reduce heart rate variability44, and are linked to catecholamine dysregulation and sympathetic activation45, ultimately heightening the risk of arrhythmia and thrombosis37,46. Additional mechanisms include impaired HDL functionality47, epigenetic modifications48, and immune activation, while emerging evidence suggests that oxidative and inflammatory pathways may also contribute to metabolic syndrome and arteriosclerosis49,50. Taken together, evidence from epidemiological, animal, and mechanistic studies strongly supports the role of particulate and gaseous pollutants in the development of HD, providing robust biological plausibility for the present findings.
Further subgroup analyses suggested that women, individuals with lower education, and rural residents were at relatively higher risk of HD associated with PM exposure. Although the interaction effects were not statistically significant, these trends point to potential population susceptibility or differences in environmental exposure. Prior studies have shown that women may be more vulnerable to pollution-related damage through oxidative stress and one-carbon metabolic pathways51; residents of areas with inadequate environmental governance or persistently high pollution levels experience greater risks of HD52; and those with lower education and socioeconomic status often have limited health literacy and protective awareness, amplifying the adverse effects of pollution53. These findings align with the stratified trends observed in this study and underscore the importance of considering population susceptibility in air pollution control and CVD prevention to enable more targeted public health interventions. On this basis, strengthening the transition to clean energy, vehicle emission control, and industrial pollution regulation is essential to reduce long-term exposure in high-risk populations and to mitigate the burden of CVD. Notably, a recent Chinese cohort study of more than 5.8 million participants confirmed the association between air pollution and CVD and emphasized the influence of lifestyle factors54. Although more modest in scale, our study focuses on middle-aged and older adults, incorporates PM₁ exposure, and employs rigorous sensitivity analyses, thereby providing complementary evidence to the existing literature.Although some pollutant–pollutant interaction terms reached statistical significance in exploratory analyses, their effect sizes were negligible (hazard ratios close to 1), lacking biological or clinical relevance. Therefore, the core conclusions of this study do not rely on these interaction results but rather focus on the robust associations between long-term single-pollutant exposures and HD risk.
Strengths and limitations
Drawing on a nationally representative cohort, this study systematically examined the associations of PM₂.₅, PM₁₀, and PM₁ exposure with HD risk and confirmed the robustness of the results through multi-pollutant models and sensitivity analyses. Subgroup analyses indicated that women, rural residents, and individuals with lower education may face elevated risks, providing valuable insights for identifying susceptible populations. Notably, this study provides nationwide epidemiological evidence on PM₁, contributing to a deeper understanding of the relationship between particulate matter and HD.
Nevertheless, this study has several limitations. Air pollution exposure was estimated from region-level averages, which may not reflect individual variability. HD outcomes were self-reported, introducing the possibility of information bias, and cross-sectional effect sizes were relatively small, limiting clinical relevance. The inconsistent associations observed for O₃ and NO₂ may reflect pollutant collinearity or spatial heterogeneity. Compared with larger-scale studies, the sample size was modest, reducing statistical power to detect weak effects or interactions. Furthermore, clinical adjudication of outcomes and advanced spatiotemporal exposure models were not applied, which may restrict the generalizability of our findings. Nonetheless, this study offers valuable complementary evidence on the association between long-term particulate matter exposure and HD in the Chinese population, highlighting the public health significance of air pollution as a modifiable risk factor. Residual confounding cannot be excluded, as individual-level data on diet, physical activity, and neighborhood environmental characteristics (e.g., greenness, traffic density) were unavailable, and meteorological covariates were not explicitly incorporated in the long-term analyses. Given the likely non-differential misclassification from city-level exposure assessment and self-reported outcomes, the observed effect estimates may have been biased toward the null.
link